Medical experts are raising serious concerns that fatalities may keep rising unless urgent measures are implemented. The infection is caused by a highly contagious bacterium that naturally resides in the human bowel.
Dr Kerrie Davies of the C. Diff Trust told Metro: “We cannot afford for more patients to be dying of this every year.”
She said people “can’t function” when struck down with the nasty bacteria.
“Patients with it tell us how scared they are. It is the worst diarrhoea that you have ever, ever had in your life,” added the expert.
Between February 2024 and January 2025, the UK Health Security Agency (UKHSA) recorded 19,239 cases of Clostridioides difficile (C. diff)—marking the highest number of infections since 2011/12. This spike in cases has raised serious public health concerns, especially given the bacteria’s potential to cause fatal illness.
Efforts to reduce C. diff rates were first implemented in 2007, leading to a significant drop in infections. However, recent statistics show a concerning reversal. From 2023 to 2024, 2,164 deaths were linked to C. diff, translating to a fatality rate of 12.9 percent. At its worst in 2007, the infection claimed over 7,000 lives in the UK.
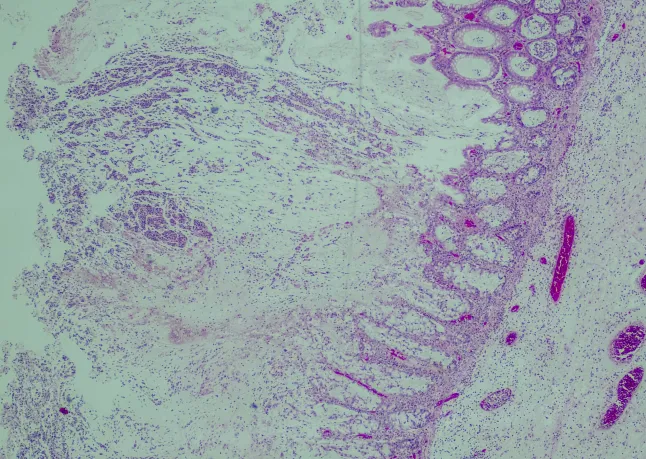
C. diff is a naturally occurring bacterium found in the human bowel and is often harmless. However, infections can develop when the gut’s bacterial balance is disrupted, often due to antibiotic use. Symptoms of a C. diff infection include severe diarrhoea, abdominal pain, and fever.
One of the most troubling aspects of C. diff is its high rate of recurrence. Individuals who contract the infection once are 25 percent more likely to get it again. If a second infection occurs, the risk of a third increases to 40 percent, and after that, the chances jump to 60 percent. With each reinfection, the risk of serious complications and death also rises.
The latest surge in cases spans across age groups and genders, but the elderly remain the most vulnerable, with a significantly higher rate of severe outcomes.
Health experts, including Dr. Davies, have voiced frustration that attention to C. diff prevention has declined since the COVID-19 pandemic. Dr. Davies warned that the medical community has lost focus, resulting in rising cases and preventable deaths.
Treating a single C. diff case can cost the NHS between £19,000 and £31,000, largely due to infection control measures like patient isolation and additional staffing. This financial burden adds further strain to an already pressured healthcare system.
Even those who recover from the infection often experience long-lasting symptoms, which can have a permanent impact on their health.
Public health campaigners are urging medical professionals to introduce routine C. diff testing for any patient presenting with diarrhoea and to cut back on the overuse of antibiotics, which remains one of the key triggers for infection.
Meanwhile, Russell Hope, UKHSA Senior Scientist and Team Lead, said: “UKHSA is working alongside partners, including NHS England, to investigate recent increases in C. difficile cases in hospitals and community settings.

“It’s likely the current rise is caused by a combination of factors, including an ageing population with multiple illnesses. Work to identify the causes is ongoing and the appropriate public health action will be taken in response to our findings.
“C. difficile is a leading cause of healthcare-associated infections (HCAIs).”
He said the “infections diarrhoea” which can “increase morbidity, mortality and hospital length of stay”.